Overview
Hair transplantation is widely considered one of the most effective and permanent solutions for hair restoration. However, many patients are surprised when they experience sudden shedding shortly after their procedure. This phenomenon, known as shock loss, can be alarming, particularly when new grafts or even surrounding native hairs begin to fall out. Understanding what shock loss is, why it occurs, how long it lasts, and how to manage it is essential for anyone planning or recovering from a hair transplant. This guide explains the science behind hair transplant shock loss, helping you distinguish between normal and concerning shedding patterns and equipping you with tools for a smooth recovery process.
Table of Contents
Understanding Shock Loss & Early Shedding
What Is Shock Loss? Definition & Key Signs
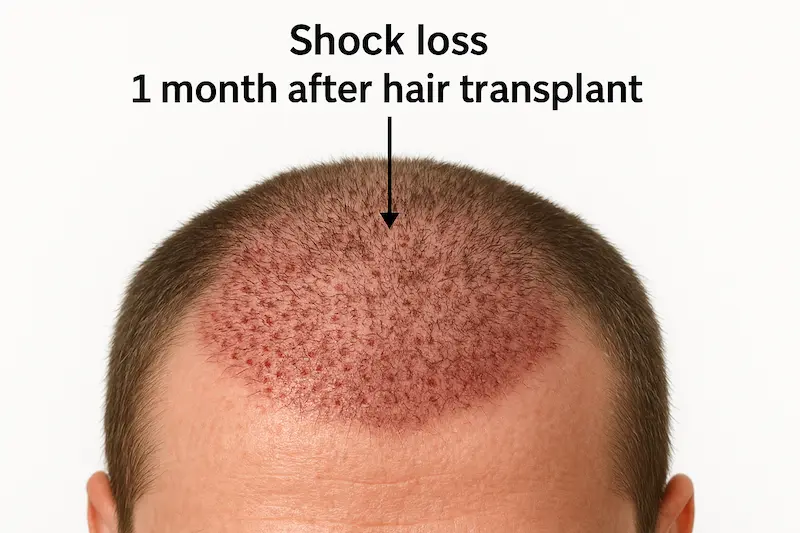
Shock loss refers to the temporary shedding of hair following a hair transplant procedure, especially within the first few weeks. It affects both transplanted grafts and sometimes the surrounding native hair. This occurs as a response to trauma inflicted on the scalp and hair follicles during surgery. The hair follicles essentially enter a resting (telogen) phase, causing the hair shaft to fall out even though the root is still viable. Typical signs include noticeable thinning in the recipient area, unexpected shedding in nearby zones, and mild scalp sensitivity. Unlike permanent hair loss, shock loss is reversible in most cases.
The term itself might sound concerning, but shock hair loss after hair transplant is a recognized and relatively common reaction that doesn’t reflect the success or failure of the transplant.
Shedding After Hair Transplant vs Telogen Effluvium After Surgery
Patients often confuse shock loss with telogen effluvium after surgery, another condition that causes sudden hair shedding due to stress or trauma. While both involve telogen-phase shedding, they differ in origin and scope. Telogen effluvium is a diffuse hair shedding pattern triggered by systemic factors such as anesthesia, nutritional deficiency, or emotional stress. It can affect the entire scalp, not just the transplanted zones.
In contrast, shock loss is typically localized and linked to physical trauma from surgery, particularly FUE (Follicular Unit Extraction) or FUT (Follicular Unit Transplantation). Both types can occur simultaneously, making it crucial for patients to consult their surgeon to determine the exact cause of post-operative shedding.
Shock Hair Loss After Hair Transplant: Why It Happens
The scalp undergoes physical stress during hair restoration. Tiny incisions, recipient site creation, and the grafting process itself can disturb blood flow and temporarily disrupt the health of nearby follicles. This physiological stress causes some follicles to stop producing hair temporarily. Grafts may shed before entering the growth phase, and native hairs in the surrounding zone may fall out in protest to the surgical trauma.
Moreover, shock loss after hair transplant is more likely in cases where the patient already has miniaturized or weakened surrounding hairs. These native hairs are more vulnerable and may not survive the trauma as well as the newly implanted, robust grafts. This explains why shedding can sometimes appear more dramatic than expected, especially if native density was already compromised.
It’s also important to remember that this type of shedding can affect both men and women. The severity and visibility of shock loss vary based on scalp condition, hair density, and the method used for the transplant. In most cases, full recovery is expected with proper aftercare.
Main Triggers of Temporary Hair Loss After FUE/FUT
Shock loss is not a random occurrence; it is triggered by specific internal and external factors, many of which are closely tied to the surgical procedure itself. Understanding these causes can help set realistic expectations and allow patients and surgeons to take preventive steps. While FUE (Follicular Unit Extraction) and FUT (Follicular Unit Transplantation) differ in technique, both can result in temporary hair loss after surgery due to several overlapping triggers.
Surgical Trauma, Vascular Stress & Follicular “Shock”
One of the most immediate causes of shock loss after hair transplant is direct trauma to the scalp. During the transplantation process, micro-incisions are made in the recipient area, and existing hair follicles near the grafted area can be affected inadvertently. This can lead to follicular shock, a condition where native or newly transplanted follicles stop producing hair temporarily as a reaction to environmental disruption.
Additionally, the process of making incisions and inserting grafts can compromise blood supply to the scalp. Vascular stress limits oxygen and nutrient delivery to follicles, making them more vulnerable to shedding. This is especially common in procedures that involve high-density graft placements or large session volumes, where the cumulative trauma is more significant. Though the transplanted roots remain intact, the visible hair shafts fall out as part of the body’s response to the surgical environment.
Inflammation, Anesthesia, Medications & Lifestyle Factors
The inflammatory response following surgery also plays a major role in triggering shock hair loss. Inflammation is a natural healing mechanism, but when it becomes prolonged or excessive, it can interrupt the hair growth cycle. The surrounding tissues swell and may exert pressure on hair follicles, pushing them prematurely into the telogen (resting) phase.
Anesthesia, both local and general, has been linked to telogen effluvium after surgery, which may exacerbate post-op shedding. Anesthesia alters the body’s metabolic balance and affects cellular activity. In some individuals, this contributes to delayed recovery and prolonged shedding after hair transplant procedures.
Certain medications prescribed during post-op recovery, such as antibiotics or corticosteroids, may also contribute to temporary hair thinning. Additionally, lifestyle factors like poor nutrition, smoking, excessive alcohol consumption, and lack of sleep can hinder the body’s ability to heal and grow new hair efficiently.
While the body typically rebounds from these temporary interruptions, awareness of these secondary factors can significantly reduce the extent and duration of shock loss.
Does Everyone Get Shock Loss After Hair Transplant?
Not all patients experience shock loss, but it is common enough that most surgeons will prepare their patients for it. The likelihood of experiencing shock loss varies based on individual scalp sensitivity, hair quality, and the chosen transplant method. Patients with healthy donor and recipient areas are generally less susceptible, while those with thinning hair around the transplant site or a history of stress-related hair issues may be more prone.
Age, genetics, and hormonal factors can also affect shock loss probability. Younger patients with active androgenic alopecia may notice more shock-related shedding, particularly if miniaturized hairs are already under stress. However, this does not indicate transplant failure. Most cases resolve with time, and new growth typically begins once the follicles re-enter the anagen (growth) phase.
Surgeons often take proactive steps to minimize this outcome by spacing grafts correctly, preserving surrounding hairs, and offering supportive treatments like PRP (Platelet-Rich Plasma) or low-level laser therapy post-operatively. These techniques can significantly reduce trauma and improve regrowth rates.
Timeline – How Long Does Shock Loss Last?
Understanding the timeline of shock loss after hair transplant helps manage patient expectations and eliminates unnecessary anxiety during recovery. While the experience varies slightly depending on procedure type, scalp condition, and patient health, most cases follow a general progression from shedding to regrowth over a 12-week period.
Week-by-Week Shock Loss Recovery Phases (Weeks 1–12)
- Week 1–2:
The scalp is still healing from the transplant procedure. During this phase, swelling, redness, and scab formation are common. Most grafts remain in place, and shedding is minimal. However, some patients may begin to notice isolated hair fall around the recipient zone. - Week 3–4:
This is when shedding after hair transplant becomes noticeably apparent. Transplanted hairs often enter the telogen (resting) phase and begin falling out. Native hairs near the transplant site may also shed due to trauma, especially in dense packing areas. This is the peak period for shock loss and can cause visible thinning or patchiness. Although alarming, this is a natural part of the healing cycle. - Week 5–8:
Shedding gradually stabilizes. The scalp’s inflammation subsides, and signs of regrowth begin at the follicular level, though it may not be visible on the surface. Some patients might experience temporary hair loss after FUE that extends beyond this period, but the shedding generally slows. - Week 9–12:
New hair begins to emerge from both transplanted and affected native follicles. The early growth may be soft, thin, and light in color. Over time, this hair becomes thicker and darker. This regrowth phase continues progressively over the next 6–12 months.
By the end of week 12, most cases of shock hair loss after hair transplant have either stopped or significantly improved. Patients typically begin seeing early-stage regrowth and can confidently assess that their follicles are reactivating.
Factors Affecting Regrowth Speed & Density
Although the standard recovery window ranges from 2 to 3 months, several factors can influence how quickly hair grows back:
- Age and Genetics: Younger individuals often recover more quickly due to better cell turnover. Genetics also determine the growth cycle speed and final density.
- Type of Transplant: FUE techniques may yield slightly quicker healing times compared to FUT, though both procedures can cause shock loss. The graft survival rate and overall trauma play a role.
- Post-Operative Care: Use of topical minoxidil, low-level laser therapy, or PRP treatments can accelerate regrowth. Following the surgeon’s aftercare protocols is critical.
- Scalp Health and Circulation: Healthy skin, strong blood flow, and absence of inflammation promote faster recovery.
- Nutritional Status: Deficiencies in iron, zinc, biotin, or protein can delay follicle recovery and prolong the resting phase.
Each person’s healing timeline is unique, but most patients regain a significant portion of their lost hair within 3 to 6 months after transplant.
When to Worry About Prolonged Shedding
While shock loss recovery is typically temporary, certain red flags may indicate deeper issues. If heavy shedding continues beyond the 3-month mark with no signs of new hair emerging, it could point to complications such as:
- Follicular damage during surgery
- Underlying medical conditions like thyroid dysfunction or alopecia areata
- Chronic telogen effluvium, unrelated to the transplant
- Excessive scalp inflammation or infection
In such cases, early intervention is crucial. Patients should consult their surgeon or a dermatologist for evaluation. Scalp biopsies, blood tests, or trichoscopy can help identify whether the follicles are still alive and capable of regrowth or if alternative treatments are needed.
Timely attention not only offers reassurance but also enables appropriate therapies to restore growth potential.
Is Shock Loss Permanent? Prognosis & Success Rates
One of the most common concerns among patients experiencing shock loss after hair transplant is whether the shedding is permanent. The fear of losing newly implanted grafts or surrounding native hair for good can cause significant anxiety during recovery. Fortunately, in the vast majority of cases, shock loss is temporary, and full regrowth is expected within a few months. This section explores the prognosis, success rates, and outcomes for both FUE and FUT procedures.
Can Shock Loss Cause Permanent Follicle Damage?
By design, shock loss involves temporary disruption of the hair cycle. The hair shafts fall out, but the follicles beneath the scalp usually remain intact and viable. However, certain situations can lead to irreversible loss, particularly when:
- The surrounding native hair is already miniaturized due to androgenetic alopecia (pattern hair loss)
- Follicles are accidentally over-traumatized during the transplant process
- There’s inadequate blood supply to the affected area
- Infections or inflammation are left untreated
- Underlying conditions such as autoimmune disorders or scarring alopecias exist
If a follicle has been severely damaged or the scalp environment becomes hostile, the hair may not grow back. However, these scenarios are rare when the procedure is performed by an experienced surgeon. Most patients regain their hair completely with proper care and healing time.
Surgeons can minimize the risk of permanent follicular injury by using refined tools, minimizing trauma, avoiding over-packing of grafts, and ensuring good post-op follow-up. Therefore, selecting a reputable clinic with skilled professionals is critical to safeguarding against long-term damage.
Comparing FUE vs FUT Outcomes
Both FUE (Follicular Unit Extraction) and FUT (Follicular Unit Transplantation) procedures are capable of triggering shock hair loss, although the risk profile may differ slightly:
- FUE Shock Loss: Due to the minimally invasive nature of FUE, the incidence of shock loss may be slightly lower, particularly in areas where native hair is sparse. However, dense packing of grafts or repeated procedures on the same zone can still induce shock-related shedding.
- FUT Shock Loss: FUT involves the removal of a strip of scalp, which can lead to greater scalp trauma and potentially higher risk of shock loss in the donor area, especially around the incision line. However, the recipient area’s risk remains similar to FUE, especially when transplanting into zones with active hair.
In both techniques, temporary hair loss after FUE or FUT is expected and follows a similar recovery trajectory. The long-term survival and success of transplanted grafts depend more on surgical skill, patient factors, and post-operative care than on the method used.
Shock Loss Recovery: Real-World Case Studies
Numerous real-world examples demonstrate that shock loss is not only common but also reversible. For instance:
- Case 1: A 32-year-old male with Norwood Class III hair loss experienced extensive shock loss at Week 3 after FUE. By Week 10, early regrowth was observed, and full density returned by Month 5.
- Case 2: A 40-year-old female undergoing frontal hairline reconstruction reported patchy native hair loss around the transplanted area at Week 4. She underwent PRP sessions starting Week 6 and regained complete coverage by Month 4.
- Case 3: A 29-year-old male with miniaturized native hairs in the crown received FUT. Partial native hair did not return due to preexisting weakness, but transplanted grafts thrived, creating full coverage by Month 6.
These scenarios illustrate that while shock loss recovery can feel unpredictable, most outcomes are favorable. Patients who adhere to recovery protocols, maintain scalp hygiene, and support healing through nutrition and non-invasive therapies typically regain all lost hair and achieve strong cosmetic results.
Preventing & Managing Shock Loss for Optimal Results
While shock loss after hair transplant cannot always be avoided, several preemptive and post-operative strategies can minimize its severity and accelerate recovery. Both patients and surgeons play a role in reducing the likelihood of extensive shedding and improving long-term outcomes. From scalp preparation to advanced therapies, proactive care leads to healthier regrowth and improved patient satisfaction.
Pre-Op Scalp Conditioning & Nutritional Support
The condition of the scalp and hair follicles before surgery strongly influences how the scalp responds to trauma. Pre-operative scalp conditioning can fortify hair health, increase blood circulation, and make follicles more resilient. Suggested measures include:
- Topical minoxidil use in the weeks leading up to surgery, which can stimulate vascular activity and enhance follicle strength.
- Gentle scalp massage or microneedling to improve microcirculation.
- Discontinuing harsh hair products that irritate the scalp.
In addition to external treatments, internal nutritional support is critical. Patients are advised to:
- Ensure adequate protein intake, essential for keratin production.
- Supplement zinc, biotin, iron and vitamin D if deficiencies are identified.
- Stay hydrated and avoid excessive alcohol or caffeine before surgery, which may compromise vascular function.
These steps help prepare the scalp for the trauma of transplantation and reduce the likelihood of widespread follicular shock.
Post-Op Care: Low-Level Laser Therapy, PRP & Topicals
After the surgery, targeted post-operative care significantly improves outcomes. One of the most effective and evidence-backed approaches is low-level laser therapy (LLLT), which enhances mitochondrial function in hair follicles and accelerates healing without side effects.
Platelet-Rich Plasma (PRP) therapy is another valuable tool in the recovery phase. By injecting concentrated growth factors derived from the patient’s own blood, PRP stimulates stem cells, supports follicle regeneration, and reduces inflammation. Studies show that patients receiving PRP after transplant report faster regrowth and lower rates of prolonged shock hair loss.
Additional topical agents like:
- Minoxidil 5% foam or solution (once approved by the surgeon)
- Caffeine-based serums or peptide sprays
- Aloe vera-based calming gels to reduce inflammation
can further support the transition from the shedding phase to active regrowth.
It’s important to note that timing is essential. Some treatments like minoxidil should be paused immediately post-op and restarted only once the grafts are secure, as instructed by the surgeon.
Surgeon Tips: Minimizing Shock Loss Risk in High-Density Sessions
Experienced surgeons apply specific techniques to minimize trauma to the scalp and reduce the chance of shock loss. These include:
- Proper spacing between grafts, which prevents overcrowding and allows better blood supply to each follicle.
- Using finer punches and blades, which reduce the amount of tissue trauma during extraction and implantation.
- Hydration and oxygenation protocols during surgery to keep follicles viable.
- Customizing recipient site angles to avoid disruption of existing native hairs.
For high-density sessions, surgeons often stagger graft placements or divide the procedure into two stages to allow the scalp to heal in phases. This can drastically lower the intensity of post-operative shedding and preserve native hair density.
Patients are also instructed to avoid:
- Direct sunlight exposure
- Tight hats or helmets
- Heavy sweating or exercise in the first two weeks
All of which can aggravate inflammation and delay healing.
With this proactive approach, both patient and surgeon work together to reduce risk, manage expectations, and encourage faster, fuller hair recovery.
FAQs
Yes, in rare cases, shock loss can affect the donor area, especially if there is trauma or poor blood circulation. This is usually temporary and regrows over time.
No. Shock loss is a normal phase of recovery, while transplant failure involves permanent graft loss. Most shock loss cases resolve with full regrowth.
Hair may grow back finer at first, but over time, as the follicles stabilize, thickness and density typically return to pre-shedding levels or better.
Yes, emotional or physical stress can trigger or prolong shedding. Managing stress through rest, hydration, and nutrition supports recovery.
Yes, mild shampoos with ingredients like ketoconazole, biotin, or caffeine can soothe the scalp and support regrowth, but always consult your surgeon first.