Overview
JAK inhibitors have emerged as a groundbreaking treatment option for autoimmune-related hair loss, especially alopecia areata. With increasing global attention and promising clinical data, these medications are transforming the way physicians approach sudden and chronic hair shedding caused by immune dysfunction. This guide explores how JAK inhibitors work, their success in clinical use, their safety profile, and why they are gaining traction as a powerful tool in the battle against hair loss.
Table of Contents
What Are JAK Inhibitors? Understanding Their Role in Autoimmune Hair Loss
JAK inhibitors, or Janus Kinase Inhibitors, are a class of medications that block specific enzymes responsible for transmitting signals involved in inflammation and immune responses. Originally developed to treat autoimmune conditions like rheumatoid arthritis and ulcerative colitis, they are now showing significant potential in managing various forms of hair loss, especially those caused by autoimmune mechanisms.
Autoimmune hair loss, such as alopecia areata, results when the immune system mistakenly attacks hair follicles. This process causes sudden bald patches on the scalp, eyebrows, and other parts of the body. Traditional treatments like corticosteroids, topical minoxidil, and immunotherapy often offer limited, temporary relief. However, JAK inhibitors offer a more targeted intervention, aiming directly at the root cause of follicular destruction.
As a result, they are now being investigated and approved for patients with moderate to severe hair loss from autoimmune origins. In 2022, the U.S. FDA approved baricitinib, a type of JAK inhibitor, specifically for alopecia areata. This regulatory milestone marked the first-ever systemic treatment authorized for this condition.
How Do JAK Inhibitors Work on the JAK‑STAT Pathway?
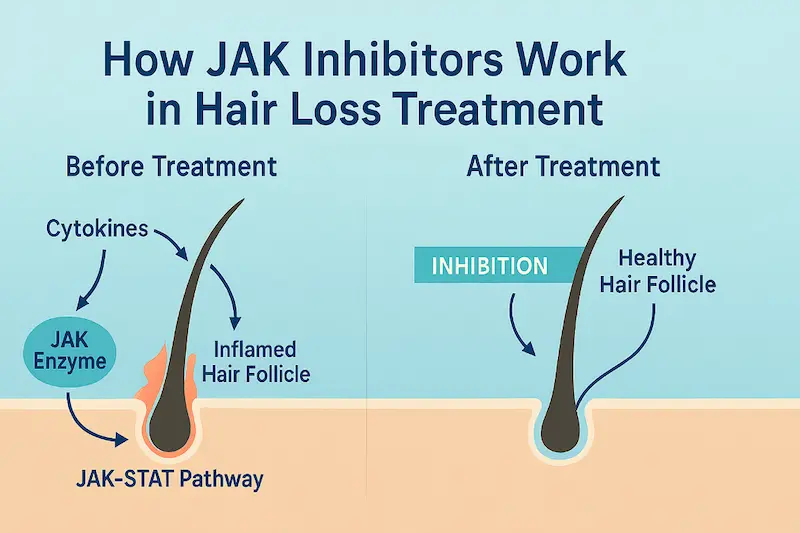
The JAK-STAT signaling pathway is a key regulator of immune activity and inflammation in the human body. When the body’s cytokines—chemical messengers that trigger immune responses bind to cell receptors, they activate JAK enzymes (Janus kinases). These enzymes then stimulate STAT proteins (Signal Transducers and Activators of Transcription), which move into the cell nucleus to alter gene expression.
This cascade is beneficial when targeting pathogens or healing wounds, but in alopecia areata, it becomes harmful. Overactive cytokine signaling results in immune cells attacking healthy hair follicles. JAK inhibitors disrupt this overactivation by blocking JAK enzymes, which stops the STAT proteins from executing inflammatory instructions. This immunomodulatory action calms the immune system and helps protect hair follicles from being targeted.
By interfering with this cycle, JAK inhibitors restore immune balance, reduce inflammation around the follicles, and allow for the resumption of hair growth.
JAK Inhibitors and Alopecia Areata: Targeting Autoimmune Attack
Among all autoimmune hair disorders, alopecia areata has shown the most remarkable response to JAK inhibitor therapy. Patients suffering from patchy hair loss, total scalp baldness (alopecia totalis), or full body hair loss (alopecia universalis) have reported measurable improvements within 3 to 6 months of treatment.
The therapeutic success lies in the specificity of JAK inhibitors. Unlike conventional treatments that broadly suppress the immune system, JAK inhibitors selectively inhibit the immune activity targeting hair follicles. This makes the treatment both effective and more tolerable for long-term use in many patients.
Furthermore, clinical trials and real-world patient experiences have shown that the degree of regrowth often correlates with the duration and severity of the condition. Those who begin treatment early tend to experience faster and more complete regrowth. However, even chronic sufferers can benefit from these therapies, making them a highly versatile option in modern dermatology.
Effectiveness of JAK Inhibitors for Hair Regrowth
As JAK inhibitors become more prominent in the treatment landscape for autoimmune hair loss, evaluating their success rate and long-term impact is essential. While they are not a universal solution for every type of hair loss, their performance in alopecia areata, in particular, has been encouraging both in clinical studies and real-world applications.
JAK Inhibitors Success Rate for Hair Growth
Multiple clinical trials have demonstrated that JAK inhibitors can significantly promote hair regrowth in patients with moderate to severe alopecia areata. In a pivotal study published in The New England Journal of Medicine, patients treated with baricitinib experienced regrowth of at least 80% of scalp hair within 36 weeks of treatment. These results represent a major breakthrough compared to traditional therapies, which often fail to reverse extensive hair loss.
Other JAK inhibitors, such as tofacitinib and ruxolitinib, have shown similar potential in smaller studies and compassionate-use programs. For example:
- In a Yale study using tofacitinib, approximately 60–70% of patients with alopecia areata experienced partial to significant regrowth.
- Case reports involving ruxolitinib highlighted dramatic regrowth in patients with alopecia universalis, the most extreme form of autoimmune hair loss.
It’s important to note that success varies depending on disease severity, duration, age, and individual immune response. Early intervention tends to yield the most favorable results.
Are JAK Inhibitors a Cure for Alopecia?
While JAK inhibitors offer substantial promise, calling them a definitive “cure” for alopecia areata would be premature. These medications effectively suppress the autoimmune attack on hair follicles, but they do not permanently reset immune function. In many cases, if the medication is discontinued, the immune system may reactivate its attack, resulting in hair loss recurrence.
In this sense, JAK inhibitors are better viewed as a long-term management tool rather than a one-time solution. Much like insulin in diabetes or immunosuppressants in lupus, they allow patients to live with the condition while keeping its most disruptive symptoms like hair shedding under control.
That said, remission is possible. Some patients retain their hair even after stopping treatment, particularly if their alopecia areata was recent or less aggressive. Ongoing studies are exploring how to extend these remissions, whether through gradual tapering, immune training, or combination therapies.
Benefits Beyond the Scalp
Another important point is that JAK inhibitors also support regrowth beyond the scalp. Many patients with alopecia areata also lose eyebrows, eyelashes, and body hair. JAK inhibitor therapy has shown effectiveness in restoring hair in these areas, providing a more holistic recovery of the patient’s appearance and self-confidence.
Additionally, because these medications have systemic effects, they may also alleviate other autoimmune symptoms or comorbidities in patients who suffer from multiple inflammatory disorders.
What Happens If You Stop Taking JAK Inhibitors?
The effectiveness of JAK inhibitors in treating autoimmune hair loss has been widely documented. However, one of the most common concerns among patients is what might happen if the treatment is stopped. Understanding this aspect is essential for anyone considering JAK inhibitors as a long-term strategy for hair regrowth.
Will My Hair Fall Out If I Stop Taking JAK Inhibitors?
In many cases, yes. Hair loss may return once JAK inhibitor treatment is discontinued, especially if the underlying autoimmune activity is still active. Studies and clinical reports have shown that some patients who stopped taking medications like baricitinib or tofacitinib experienced a gradual return of hair shedding within weeks or months.
This recurrence occurs because JAK inhibitors suppress the immune response but do not eliminate the root cause of the autoimmune condition. When the suppression ends, the immune system may resume its attack on hair follicles. This is why dermatologists often caution patients that stopping the medication abruptly can reverse the progress made.
However, not everyone will experience the same outcome. Some individuals, especially those with milder or newly diagnosed alopecia areata, may maintain hair growth after cessation. These cases are less common but show that long-term remission is possible under the right conditions.
Duration of Treatment: How Long Should You Take JAK Inhibitors?
There is currently no universally accepted timeline for how long JAK inhibitors should be taken for hair loss. Most dermatologists recommend continuing treatment as long as the patient is experiencing benefits and not suffering from side effects. In clinical trials, patients often took the medication for six months to one year to achieve full regrowth.
Longer treatment durations may be necessary for patients with more severe or long-standing alopecia areata. Doctors usually monitor hair density, immune markers, and patient response before adjusting or discontinuing the medication. In some cases, they may advise tapering the dose gradually instead of stopping it all at once.
Patients must work closely with their dermatologist to determine the ideal treatment timeline. Regular follow-ups and lab work can help track progress and minimize risks during transition phases.
Can You Maintain Hair Growth Without Continuous Medication?
In select cases, yes. Some patients maintain hair regrowth even after stopping JAK inhibitors, particularly those who responded quickly and completely to treatment. Factors that influence sustained results include age, severity of the condition, response speed, and overall immune health.
Combining JAK inhibitors with supportive therapies such as topical minoxidil, microneedling, or corticosteroids may help extend the benefits. Additionally, adopting an anti-inflammatory lifestyle, focusing on stress management, sleep quality, and a nutrient-rich diet may help the immune system stay in balance.
However, there is currently no reliable method to predict who will sustain hair growth without ongoing medication. Patients should be prepared for the possibility of needing long-term or intermittent treatment to manage their condition effectively.
JAK Inhibitors Side Effects and Safety Considerations
While JAK inhibitors are proving to be effective in restoring hair in autoimmune conditions like alopecia areata, they are not without risks. Like any systemic medication that modulates the immune system, JAK inhibitors require close monitoring and patient education. Understanding the possible side effects and knowing who may not be suitable for these treatments is a vital part of responsible care.
Common Side Effects of JAK Inhibitors
The most frequently reported side effects of JAK inhibitors include mild symptoms that can be managed during treatment. These may include:
- Headaches
- Nausea
- Upper respiratory infections such as colds
- Fatigue
- Acne or skin blemishes
These symptoms are usually temporary and subside as the body adjusts to the medication. In many cases, these effects are mild and do not require discontinuation of therapy.
Some patients may also experience slight elevations in cholesterol or liver enzyme levels. These can be detected and managed through routine blood tests, which are typically scheduled at regular intervals throughout the course of treatment.
Serious Risks and Long-Term Safety
Although most patients tolerate JAK inhibitors well, there are some serious risks associated with long-term use. These include:
- Increased risk of infections such as tuberculosis, shingles, or pneumonia
- Blood clots, particularly in the legs or lungs
- Elevated risk of cardiovascular events such as heart attack or stroke
- Rare risk of certain cancers or lymphomas with prolonged immune suppression
These risks are more common in patients who have other health conditions, are over the age of 50, or have a history of smoking or cardiovascular disease. This is why JAK inhibitors are generally prescribed with caution and under strict supervision, especially in higher-risk individuals.
The U.S. Food and Drug Administration has issued warnings regarding the use of JAK inhibitors for autoimmune conditions, emphasizing the need for patient selection, risk assessment, and long-term monitoring.
Who Should Avoid JAK Inhibitor Treatment?
Not everyone is a suitable candidate for JAK inhibitor therapy. Patients with the following conditions may be advised to consider alternative treatment options:
- History of cancer
- Current or recent serious infections
- Blood clotting disorders or cardiovascular disease
- Liver disease or impaired liver function
- Pregnant or breastfeeding women
Doctors typically perform a comprehensive health evaluation before prescribing JAK inhibitors. This includes reviewing medical history, current medications, and lifestyle factors that could increase the risk of side effects.
It is also important to avoid combining JAK inhibitors with other strong immunosuppressive drugs unless specifically instructed by a healthcare provider.
Monitoring and Follow-Up
Patients on JAK inhibitors require regular check-ins with their healthcare team. Blood tests are typically performed before starting the medication and repeated every two to three months. These tests help assess:
- Liver and kidney function
- Cholesterol levels
- Blood cell counts
- Signs of inflammation or infection
In addition to lab monitoring, patients are encouraged to report any symptoms such as fever, shortness of breath, chest pain, or unusual bruising. Early detection of complications can make treatment safer and more effective.
Who Should Consider JAK Inhibitors for Hair Loss?
JAK inhibitors are not intended for every type of hair loss. They are highly specialized medications, most suitable for individuals suffering from autoimmune-driven hair loss, particularly alopecia areata. Understanding who benefits most from this therapy helps set realistic expectations and improves treatment outcomes.
Ideal Candidates for JAK Inhibitor Therapy
The patients most likely to benefit from JAK inhibitors are those with:
- Moderate to severe alopecia areata
- Rapid or sudden patchy hair loss
- Alopecia totalis or alopecia universalis
- A history of poor response to traditional treatments like corticosteroids
- Strong motivation for regrowth and willingness to undergo long-term treatment and monitoring
Those with early-stage alopecia areata may experience faster and more complete regrowth. Patients who begin treatment within the first few months of symptom onset often report the most dramatic and lasting improvements.
In contrast, JAK inhibitors are not recommended for individuals experiencing hair loss due to genetic causes such as androgenetic alopecia, unless future research expands their indications.
Future of Hair Loss Treatment with JAK Inhibitors
JAK inhibitors represent a shift in how medical professionals understand and treat certain types of hair loss. Rather than applying surface-level treatments that stimulate follicles externally, this class of medication addresses the internal autoimmune dysfunction responsible for follicle shutdown.
Researchers are now exploring topical forms of JAK inhibitors that may deliver localized treatment with fewer systemic risks. Early trials using topical ruxolitinib and tofacitinib have shown promise in small groups of patients. If successful, these alternatives could offer patients safer, easier-to-manage options with comparable results.
Additionally, combining JAK inhibitors with regenerative techniques like platelet-rich plasma therapy or low-level laser therapy may enhance their effectiveness. These developments hint at a future where autoimmune hair loss can be managed with highly personalized, multi-modal treatment plans.
As more data becomes available and pharmaceutical advancements continue, JAK inhibitors are expected to play a central role in the dermatological toolbox for autoimmune hair disorders.
Final Thoughts for Patients Considering JAK Inhibitors
For patients experiencing the emotional and physical toll of alopecia areata, JAK inhibitors offer a scientifically backed, targeted option that addresses the root cause of hair loss. These medications have helped many individuals achieve full or near-complete regrowth, restoring both their hair and self-confidence.
However, they are not a one-size-fits-all solution. Success depends on many factors, including how early treatment begins, the severity of the condition, and the patient’s overall health profile. Long-term use requires commitment, close monitoring, and awareness of potential risks.
Before starting therapy, patients should consult with a dermatologist experienced in autoimmune hair loss and immunosuppressive treatments. Through informed decision-making and regular follow-up, many patients find JAK inhibitors to be a life-changing intervention in their journey to hair recovery.
FAQs
No, JAK inhibitors are not effective for androgenetic alopecia. They target autoimmune-related hair loss, not hormone-driven conditions.
Some studies have explored their use in children, but pediatric use requires careful supervision by a specialist and is not yet widely approved.
Yes, JAK inhibitors are prescription-only medications and must be prescribed by a licensed dermatologist or healthcare provider.
Topical forms are still in the experimental phase. While early results are promising, they may not yet match the effectiveness of oral treatments.
In some cases, yes. Dermatologists may combine them with topical minoxidil or PRP therapy, but this should be done under medical guidance.